Welcome to 2026 — the year we decide discomfort is so last year.
We’re done pretending that tightness is “just part of getting older.” We’re done negotiating with knee twinges like they’re unionized. And we’re done trying to out-stretch chronic pain with YouTube videos recorded in 2014.
This is the year we reclaim our bodies, our mobility, and our confidence — and at Uncommon Physical Therapy, we’re ready to walk (and squat, and lunge) that journey with you.
1. Pain Isn’t a Personality Trait — And It Doesn’t Belong in 2026
We say it all the time:
You don’t have to live with pain. And you definitely don’t have to live less because of it.
The truth is, most people tolerate discomfort far longer than they need to. But outstanding, hands-on, expert physical therapy remains the most powerful — and underrated — tool for getting your body back to peak performance.
And this is exactly where Uncommon Physical Therapy shines.
2. Uncommon Physical Therapy Success: What Makes Us Different
Here’s the part where we get honest.
Most outpatient orthopedic physical therapy clinics settle into a “good enough” rhythm — quick sessions, crowded schedules, generic exercise printouts, and the classic “just keep doing these at home” speech.
But at Uncommon Physical Therapy, “good enough” is… well, way too common.
We exist to change the expectations of what physical therapy should feel like.
That’s why:
- We value the time and financial commitment you make to be here.
- We believe in-person physical therapy is unparalleled in driving real, lasting results.
- We give you the highest level of commitment, every visit.
- And our mission is simple:
Help you achieve your unique goals — uncommonly well.
Our ethos sums it up best:
“Success is uncommon and not to be enjoyed by the common man.”
We hold ourselves to a higher standard because we want to be a true part of your success story — not just another stop on your healthcare tour.
3. UNCOMMON COURTESY: Where Your Experience Actually Matters
Here’s something refreshing:
When you walk into Uncommon Physical Therapy, you are the priority.
Not your diagnosis.
Not your insurance code.
Not your therapist’s packed schedule.
You.
While most PT clinics promote the long list of conditions they treat, they often forget the most important thing:
the patient experience.
At Uncommon PT, you can expect:
✨ Meaningful one-on-one time with your therapist every single visit
✨ Evidence-based treatment backed by over 20,000+ client visits (10+ years of consistent care)
✨ Personalized solutions, not cookie-cutter protocols
✨ A team that actually listens — because this is your one visit today, not our fifth
Your body isn’t a template, and your treatment shouldn’t be either.
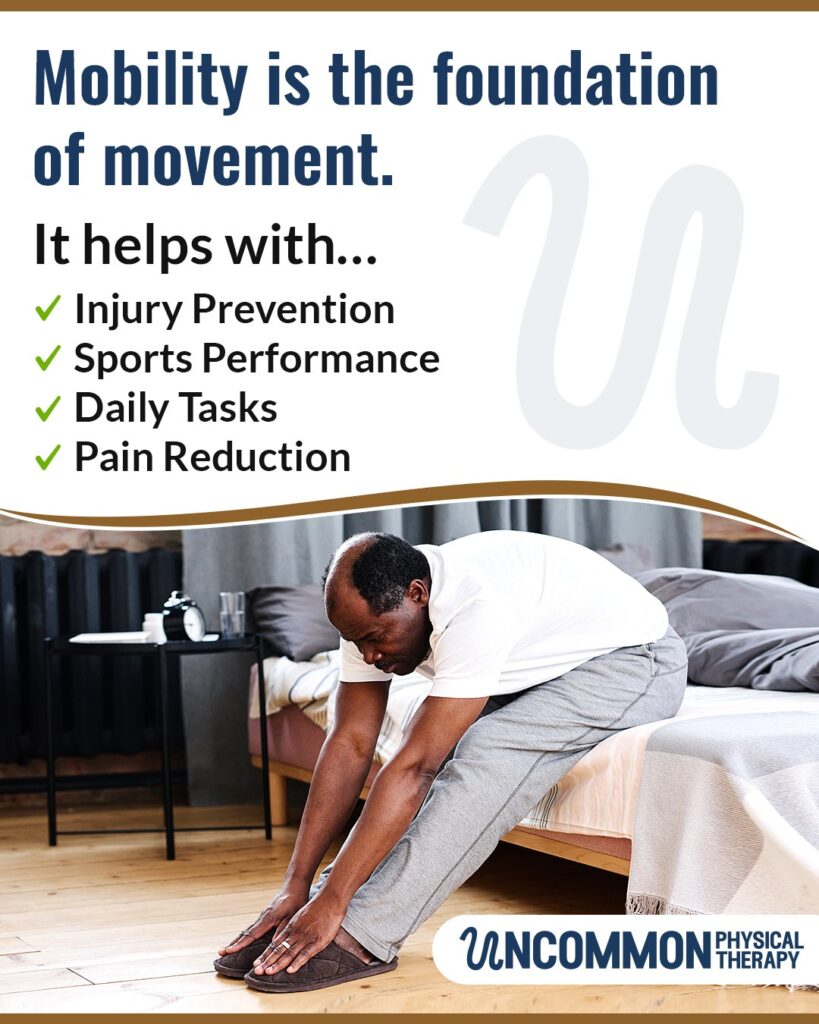
4. Mobility Is Your 2026 Superpower
Reaching overhead without wincing?
Getting off the floor without plotting your next move like a NASA launch?
Sleeping through the night without that one hip waking you up?
Yes, these are superpowers — and yes, you can have them.
With targeted manual therapy, personalized corrective exercises, and expert guidance, your body can regain the mobility you forgot you were capable of. When movement becomes effortless, everything else becomes possible.
5. Shoulder Pain? Knee Pain? Back Pain? 2026 Says “Not Today.”
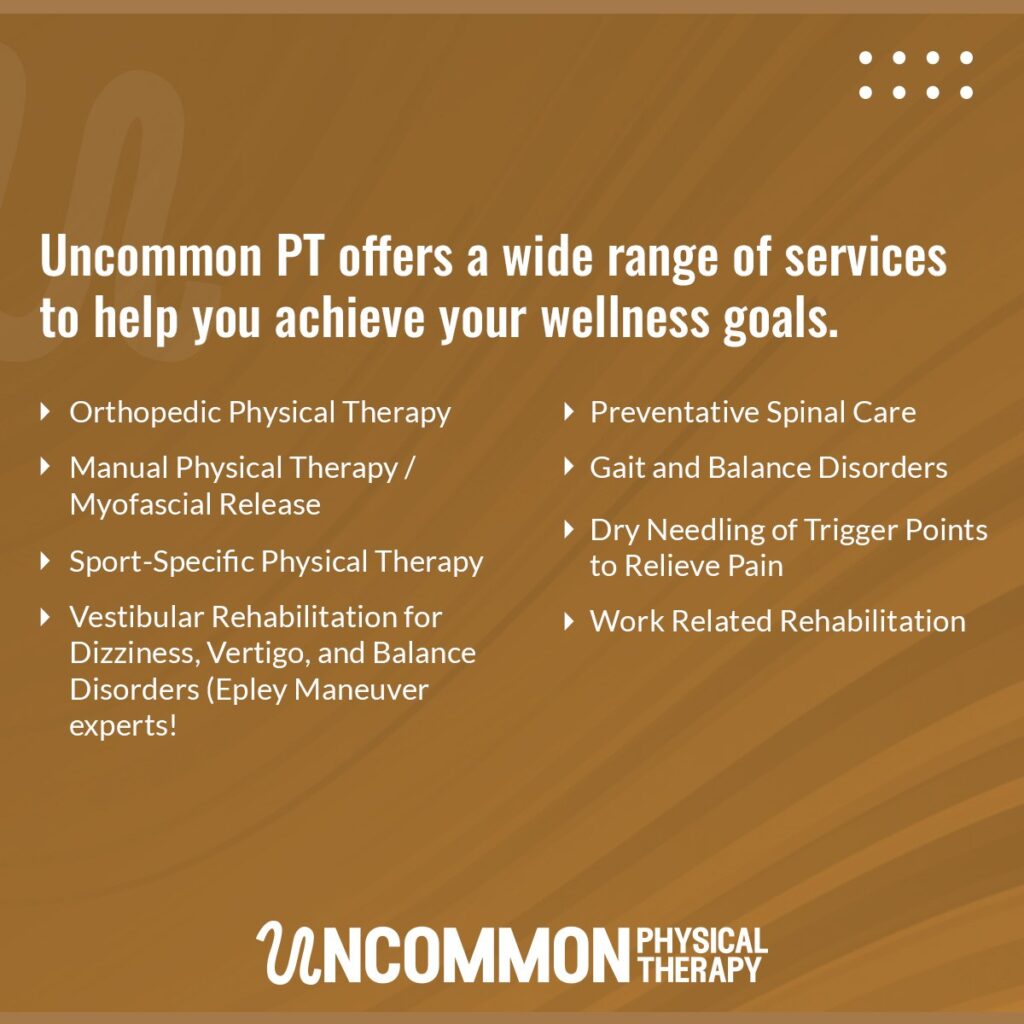
From nagging tendons to stubborn shoulders to post-op recovery, our team treats it all — but more importantly, we treat you.
If shoulder issues are holding you back, our Shoulder Physical Therapy services are specifically designed to restore strength, mobility, and confidence without unnecessary procedures or long-term medication dependency.
Whether you want to get back to lifting, swimming, throwing, or simply taking off your jacket without strategizing your escape route, we’ve got you.
6. Meet the Team That Makes It All Uncommon
Your success is built by the people who guide you — and we’re proud of the team behind the transformation:
Davis – Owner
Vision-driven, detail-oriented, and committed to reshaping what physical therapy should be.
Davis believes in pairing clinical excellence with a patient experience that feels human, supportive, and truly effective.
Cassie – PT, DPT
Movement expert, problem-solver, motivator.
Cassie brings a blend of compassion, precision, and clinical insight that helps patients feel both cared for and capable.
Justin – PT, DPT
Clinical expertise meets creativity.
Justin has a gift for identifying root causes, tailoring solutions, and empowering patients to move with confidence — often sooner than they expect.
This is the team that treats your goals as if they were their own.
7. 2026: The Year You Choose “Uncommon” for Your Health
Let’s make this the year you:
- feel stronger
- move easier
- ditch the daily discomfort
- stop accepting pain as “normal”
- and finally invest in a healthier, happier you
Because success is uncommon — and you deserve it.
Start 2026 With Uncommon Strength, Uncommon Health, and Uncommon Support
📍 Uncommon Physical Therapy
6842 Carnegie Blvd, Suite 205
Charlotte, NC 28211
📞 Call Us: (704) 803-8038
📧 Email: Info@UncommonPhysicalTherapy.com
If you’re ready for real, lasting change — the kind that transforms your health instead of just treating symptoms — we’re here.
Start 2026 strong.
Start it pain-free.
Start it Uncommon.